Death and Grief in the shadow of Covid19 – June 2020
The last few months have been extraordinary with the spread of Covid19 and the many changes to our lives, some temporary and some maybe for a long time to go.
Noone’s life has been untouched and I can’t help but be moved when I hear about the deaths during this time, whether Covid19 related or not, and the grief experienced by the people left behind. The harsh reality of the death of someone close and cherished has been compounded by not being able to go and see people, stand with them or hold them in their grief.
In March I lost a very dear friend who I’d known for over 30 years and was not able to attend the funeral or see her husband and family which added negatively to the feelings of grief.
Just this week I was saddened to hear about the death of Michael Seres a lovely person, innovator and patient leader. I only met him once but talked about his work and inspiration many times.You can read more about his life here from Marie Ennis-O’Connor. Tribute to Michael Seres
The loss of a much loved mother or father has been even closer in my mind as the sunny May this year replicated the one 23 years ago when my mother was dying and I’ve written about that before here. A good death? Yesterday June 2 would have been my father’s birthday but he sadly died in July 15 years ago.
Someone I follow on Twitter let us know that her mother had died and is wrestling with the shock and profound loss that follows and in sharing some of her feelings she asked this:
‘What do you do when almost every thought is “I’ll tell Mum about this….this will make Mum laugh..”
Of course no one has a definitive answer but we all shared some of our experiences which I hope will help her, maybe not right now but in times ahead when the shock wears off. This still happens to me from time to time when pre-lockdown I was out shopping and I’d see something and think I’ll get that for mum or dad as they’ll love that and just momentarily forget they are dead, a quick swallow of the lump in my throat follows.
But mostly I try to use the good memories I have and talk about them with family and friends. I feel I have a duty to pass these onto the younger generation in our family my niece and nephew, who were quite young when my parents died.
I want them to know a bit about their lives. The struggles and the joys – but more importantly the love they had for me and my brother. They encouraged us and let us get on with our lives but we knew if we were ever stuck or needed someone to have our backs they would be there for us.
I do tell my niece and nephew and their partners anecdotes, as I did when they were growing up, and sometimes I know I forget and repeat a story and my niece will smile wryly and say ‘Oh is this the story when grandma went and ……’ and I think oh good she remembers!
I was going through some old photographs recently to put together a photobook for my niece’s birthday and I enjoyed seeing many reminders of the past with my parents. It struck me that of course I’ll always remember and miss them but their most precious legacy was that I knew I was always loved.
I think that is why when you lose parents the grief can be overpowering because you cannot return the deep love you had for them anymore.
I think this quote about grief, attributed to Jamie Anderson, went some way to understanding what I went through when I was grieving.

I think over the years since my parent died the love I had for them is still there, of course, but channelled now into family and friends along with hopes for the future, even though currently life seems very uncertain.
That love is their legacy to us and the generations that follow.
Work-life balance for working carers and employers
Since April 2018 I’ve been working with the Greater Manchester Health & Social Care Partnership as Independent Chair of the Greater Manchester (GM) Carers Strategic Group. This group is overseeing the work underway to improve support for carers across the 10 localities which make up Greater Manchester. My first blog about this work and my motivation to improve support was published during Carers week in June 2018. Carers week 2018
Today, November 30 2018, is Carers Rights Day and I’d like to share with you some thoughts behind the development of an excellent publication called the Working Carers Toolkit for employers which is being launched today. GM supporting employers to support working carers
 If you Google ‘Work life balance’ lots of advice appears as to how to achieve a good balance of your time and energy in work and in your personal life. There are plenty of tips for managing your time well at work and not letting work invade your personal time and other challenges in people achieving a good work-life balance
If you Google ‘Work life balance’ lots of advice appears as to how to achieve a good balance of your time and energy in work and in your personal life. There are plenty of tips for managing your time well at work and not letting work invade your personal time and other challenges in people achieving a good work-life balance
If you then factor in that 1 in 9 of the workforce across the UK combine caring for a loved one with paid work out of the home then the problem of trying to achieve any kind of balance is magnified. In Greater Manchester it is estimated that around 142,000 employees (ONS Census, 2011) have additional, unpaid, caring responsibilities in the home.
It is not surprising that many working carers end up exhausted or become ill themselves trying to juggle the demands of paid work and caring, never mind having any kind of personal life themselves. Many will eventually drop out of paid work altogether and Carers UK reported in 2017 that in their survey, 4 out of 10 carers had given up paid work completely to care for a loved one at home. Employers are also losing people with significant, valuable skills and experience which are then lost to organisations and the overall economy.
Every carer’s situation and job requirements are different and individual but there is no doubt that there are some things that employers can do to enable them to retain experienced staff and for staff to feel supported in juggling their job and carer responsibilities such as:
- Use of technology to work from home or dial into meetings where short notice caring responsibilities prevent them coming into the office
- Being able to have access to a telephone and privacy to make calls related to their caring role
- Flexibility in working arrangements around medical appointments for the person they care for, taking time off and then working replacement hours at a later time
I well remember the feelings of guilt of often leaving work early in Manchester on Fridays and driving down to Worcestershire to support my father in caring for my mother and then leaving at 5.00am on Monday morning to drive straight back into work.
I worried about being preoccupied at work due to stress and worry as my mother was approaching end of life care and was I doing enough to help my father and mother in the limited time I could physically be there with them both? In those last 3 years of my mother’s life there were also many emergency dashes up and down the M6 as my mother experienced crises, emergency admissions to hospital and where her life hung in the balance on many occasions. I juggled leave to make up some of the shortfall, made frequent phone calls in the times I wasn’t physically there with them and generally muddled through some of the worst times of my life.
Each working carer has their own story and challenges to relate and many like me will enjoy their jobs and want to keep them. Equally employers want to retain their staff and many can be unaware of the often hidden struggles that many staff experience until they reach crisis level and decide to leave.
Supporting working carers in Greater Manchester
As part of the work underway across Greater Manchester to improve support for carers this Friday November 30 – Carer’s Rights Day- sees the launch of the GM Working Carers Toolkit – interactive version for employers which provides support for employers using insight from the association of Directors of Adult Social Services in England(ADASS) and what working carers have related from their experiences.
In summary the toolkit describes, and evidences why supporting working carers is both good for carers and good for business.
In the toolkit practice tips, suggestions and resources for employers are provided which draw on reports based on feedback from working carers in Greater Manchester through the work of the Greater Manchester Health & Social Care Partnership, from Carers UK, Chartered Institute of Personnel and Development(CIPD) and ADASS.
A key part of the support that will be available in Greater Manchester will be the opportunity to take advantage of the umbrella membership of Employers for Carers from Carers UK, for Local Authorities, partner organisations and Chambers of Commerce to enable Small and Medium sized enterprises(SMEs) to gain free access to the wealth of resources available.
A customised website for Greater Manchester is being set up which also has provision for each locality to have their own pages too so that initiatives specific to different areas can be tailored to them as well as offering future opportunities to share experiences and learning across the region.
So do take a look at the information available from November 30 2018, and if you’re an employer in Greater Manchester, I’d encourage you to take advantage of the Greater Manchester Working Carer Toolkit for employers (print version) and especially check out the simple, short, self- assessment tool at the end to reflect on what you currently know, and do for your employees who are carers.
Remember supporting working carers is: 
- GOOD FOR CARERS and
- GOOD FOR BUSINESS
If you want to hear more about the work underway in Greater Manchester to improve support for carers you can get a brief overview from a recent BMJ podcast where I talked with Anya de longh BMJ Patient Editor here: Carers Need a Voice
A bump in the road (An everyday tale of self-managing long-term conditions and being knocked off course).
The ‘eye make-up’ moment and why I’ve not blogged in a while.
I bought myself some new eye make up last week and was trying to remember why I’d stopped wearing it and when was the last time I’d bought any. 
Then it came to me it was another thing that had slipped off my daily routine due to the effects of the car crash back in June 2016 when I’d been hit from behind at a roundabout.
At the time, apart from being initially shocked and shaken up my mind had been taken up by how getting my car repaired, dealing with insurers, getting a replacement car in the interim etc would take loads of time and effort to get through. I was grateful that the person who hit me had apologised straight away, accepted blame and was kind enough to ask how I was as I shakily got out of my car.
Equally I had almost expected a few bruises along with my existing arthritic, neurological and gastrointestinal conditions flaring up which they did with style and kept going for months. What I wasn’t expecting was a new acute condition to join in. I was in more pain than usual due to the arthritic flares but the increasing pain in my shoulder was new and quickly got my attention above all the rest as it reached excruciating level.
To cut a long story short my shoulder had been damaged and very quickly became agonisingly painful and unmoveable. So after investigations, an interim procedure and advice from an orthopaedic surgeon I ended up having surgery on my shoulder 7 months after the accident. I had a good result from the surgery but now have some permanent loss of movement and strength and some residual, albeit generally low-level pain.
So what has eye make up got to do with the car crash and my shoulder?
It’s only now, 18 months since the accident, that my life is nearly getting back to my normal that I’ve realised just what impact that bump had on my day to day life.
As my shoulder increased in pain and lack of movement everyday functioning became more and more difficult. For example getting dressed and undressed with only one functioning arm became a more time consuming and painful part of my day than usual.
A challenge too far?
One good thing about already having chronic long term conditions is that I live on one level in an apartment and have some adaptations such as pick up sticks and rails in the bathroom etc. But I quickly realised that being down to only one functioning arm was almost a challenge too far.
Additionally the added levels of pain contributed to the overall fatigue levels I experience normally so I had to prioritise even more to get through the day.
Reflecting back now I realise that I prioritised basic needs and functions in order to maintain the part time work I do and gradually nearly everything else dropped off my radar.
The ‘everything else’ included things I love to do such as swimming, writing, visiting friends, family and places and going to the theatre. Most of these activities became too painful and/or too tiring to accomplish easily and indeed became chores instead of relaxing and restoring times.
Adjustments to daly routine
I pared down my essential daily routines too which is why putting on eye make up stopped, as I couldn’t use my left hand higher than my waist. Even what I ate changed to some degree as I could only use one hand reliably and safely and even now have to be careful, as my left arm has not regained full strength or movement.
When I wasn’t working, and as I said before I can only work part time, I was often flat out on my sofa or in bed early as I was so tired from the additional effort to keep going and the added pain which was heaped on my existing normal pain levels.
It’s only now as I get back to some semblance of ‘my normal’ and I’m gradually picking up some activities that I realise just how much this ‘bump in the road’ knocked me off course in terms of self managing well and even to some extent socially isolated me as I stopped being able to do things easily and stayed in more on my own. I say this cautiously as I didn’t have an all singing all dancing social life before the bump but I have missed the things I did manage to do which connected me with other people.
I’m grateful this bump in the road wasn’t life threatening but it certainly wasn’t life enhancing! I’m also grateful for the support of those friends who like me live with chronic conditions and who just understood and didn’t mind me whingeing from time to time. Their sense of humour, always quirky, certainly helped a lot- thanks people – you know who you are.
 As I’m picking up slowly now I’m reflecting back and wondering could I have managed better? Should I have tried harder to hang onto doing social stuff? I think I did try but ran out of options as I lost function and pain was overwhelming.
As I’m picking up slowly now I’m reflecting back and wondering could I have managed better? Should I have tried harder to hang onto doing social stuff? I think I did try but ran out of options as I lost function and pain was overwhelming.
Most of the advice about living with pain conditions from the NHS, or specific charities such as Arthritis Research, which I have found useful before didn’t really help me much this time as I’ve lived with deteriorating conditions for more than 20 years now.
How do you manage ‘bumps in the road’?
So I’m interested to know your experiences if you are managing different conditions and how you get on when something else disrupts your ‘normal’ routine? Is letting go of social stuff just part of managing? Or have you discovered better ways to get through life’s diversions and road bumps?
For information
NHS Choices
Living with pain, information about different health conditions, self care tips,
https://www.nhs.uk/Livewell/Pain/Pages/Gettingphysical.aspx
Arthritis Research
Living with long term pain and daily life
Keeping track of my life & health history – online patient access to records
I’m wondering what records you keep personally, or can access online, to help you keep track of your life and I’m especially thinking about personal health?
Keeping track of my appointments, medications, symptoms
As some of you know my health took a downturn in my mid 40s and since then I have been managing a few Long Term Conditions. As I became a more experienced patient I realised that no one NHS organization had the full record of my health history and so I began to keep a simple record on my laptop that detailed dates of appointments, which clinician I’d seen, what had been said (that I could remember) and if there was any follow-up or monitoring to do.
I did this just for my own peace of mind as I was always asked what medication I was taking, what operations/procedures/blood tests/results I’d had and when, and what my current symptoms were etc.
As my history became more complex I used my own record as an aide memoire for me to take with me to appointments and it also came in useful as a briefing sheet for any new consultants/clinicians I met.
Then I heard that nationally the NHS was going to give patients access to the records that were kept by GPs and I thought great that will be an enormous help.
Online access to shopping and banking
As I have become physically disabled with arthritic and spinal problems I have come to use online services for many aspects of my life including shopping and banking. I started cautiously with banking online over 15 years ago and now the only thing I can’t do online is take money out or pay in cheques!
I’m not the only one as in 2015 the people who use internet banking was around 56% according to the Office for National Statistics.
And before anyone says it’s too much for the more advanced in age the British Banking Association(BBA) reported in the Way We Bank Now that there are millions of “Silver Surfers” using mobile and internet banking with nearly 2.3 million people aged between 70 and over 100 years old using internet banking. The study also shows that more than 450,000 customers over 60 are harnessing banking apps on smart phones, iPads and other tablets.
Now the banking industry made these changes so that their customers could more easily use their banking services and keep track of their finances.
There is no doubt that internet use has changed the way many people manage different aspects of their lives. In 2015 the Office for National Statistics said that the internet was accessed every day, or almost every day by 78% of people in Great Britain with online shopping and use of services being the most popular of their use. And that 86% of households in Great Britain had internet access.
So back to health.
You can imagine how delighted I was to hear about the National NHS Patient Online programme and I quickly signed up for the facility to order my monthly repeat prescriptions online which saved me monthly trips to the GP surgery and saved receptionist time receiving paper requests and finding my prescription scripts for me.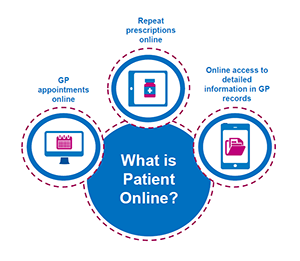
From the 31st March 2016 all GP practices across England should be offering online services to their patients which include, ordering repeat prescriptions, booking appointments online, access to summary information (immunisations, allergies, medication) test results and lastly access to detailed coded information held in patients’ records.
This seemed to me to be really good news for people and especially for those, like me, with Long Term Conditions who want to be active in self managing their life whenever possible and if support is needed can do this in partnership with healthcare professionals.
I must confess that I was a bit disappointed when I did get finally get access to the coded information in my records, a few weeks ago, as I didn’t get my past history so I will only have access to future events. Thankfully I still have my own record to rely on and hope that future generations will get this straight away so they will have a chronological record to use.
Who knows about this and how do you get access?
This seems to be a problem in some places where not many patients are aware that online services are available or what this could mean to them personally. If they do know people report that it can be difficult to find out how to do this at their own surgery, as information doesn’t appear to be always readily, or easily, available.
Here are some Frequently Asked Questions for patients from NHS England.
https://www.england.nhs.uk/wp-content/uploads/2016/03/nhs-po-patient-faqs.pdf
Equally it seems that some GP practices do not yet see the potential of how online services could free up time for them and more importantly enable their patients to be more informed and self-managing partners.
Frequently Asked Questions for GP practices
https://www.england.nhs.uk/wp-content/uploads/2015/11/po-faqs-practices.pdf
There has been a lot of publicity nationally in England from the Patient online team and support is available for practices where there are local needs but this isn’t enough as there still appears to be a huge gap between what is ‘technically’ available and what is promoted to patients and made easily available at practice level.
For me personally I can only see benefits and a friend of mine Ingrid Brindle has built up  her knowledge over a few years of having full access to her records at the forward thinking Haughton Thornley Medical Centre in Hyde (led by Dr Amir Hannan) Greater Manchester where she is Chair of the Patient Participation Group. Listen to Ingrid talking about her experiences at The Kings Fund in 2014.
her knowledge over a few years of having full access to her records at the forward thinking Haughton Thornley Medical Centre in Hyde (led by Dr Amir Hannan) Greater Manchester where she is Chair of the Patient Participation Group. Listen to Ingrid talking about her experiences at The Kings Fund in 2014.
If you’re still not sure and want to know more you can watch, and listen to, these short case studies snapshots, which include different views from GPs, practice managers, receptionists and more patients. You can hear again from Ingrid and just below Ingrid is another colleague of mine Trevor Fossey who talks about how useful it is to him and his wife, who he cares for, to have online access to their records.
https://www.england.nhs.uk/ourwork/pe/patient-online/learning-so-far/case-studies/
For me having online access to my records, test results, medications, and prescription ordering isn’t really about gadgets or Information Technology (IT).
It’s about me being responsible and empowered in being as informed as I can be to make decisions about my most valuable asset, my health.
5 ingredients for co-production
I’m really pleased to be re-blogging this piece written by Shahana Ramsden who is the Senior lead for co-production at the Coalition for Collaborative Care. http://coalitionforcollaborativecare.org.uk
I am member of the co-production group which is made up of a wide range of people with Long Term Conditions(LTCS) and carers of people who have LTCs. The main assets of the group, who all have many skills and expertise, is the passion each individual has to make a difference in health and social care which is the reason that drives me.
I learn something new from each individual every time we meet or work together but must say that I have benefitted the most from Shahana’s lead, direction and diplomacy. Thank you Shahana- it is a pleasure to re-blog your piece on co-production here.
Shahana Ramsden blogs for us today on her 5 ingredients for co-production. She is the Senior Co-Production Lead NHS England and the Coalition for Collaborative Care (Co4CC). Shahana’s 29 year career includes supporting co-production with people who use services and carers and leading equalities programmes. Prior to her role with NHS England and Co4CC, Shahana worked as a Patient and Public Voice Manager for NHS England’s Patient Online programme. Shahana has been recognised by the Health Service Journal as a BME pioneer and was highlighted as one of 100 virtual change activists for Health and Social Care through NHS IQ (The Edge).
Working in Co-production with patients, people who use services and carers can be simultaneously simple and complex. It is messy, not linear. When it works well we have to prepared for a change in culture so that we avoid fitting people into boxes and are prepared to position the organisation…
View original post 995 more words
Person Centred Care and coproduction – the ‘get real’ factor.
 This year I’m attending EXPO 2015 as a member of the People’s Panel which is a group of people who are patients or carers and who have lived experience in learning to deal with their own Long Term Conditions or as a carer, and who have also become expert in navigating the sometimes complex world of health and social care.
This year I’m attending EXPO 2015 as a member of the People’s Panel which is a group of people who are patients or carers and who have lived experience in learning to deal with their own Long Term Conditions or as a carer, and who have also become expert in navigating the sometimes complex world of health and social care.
The fact that the planning for EXPO has included patients and carers is demonstrating the drive and commitment of NHS England and the Five Year Forward View to develop “..a more engaged relationship with patients, carers and citizens so that we can promote wellbeing and prevent ill-health”. https://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf
This new relationship will be exemplified by members of the People’s Panel to show how working together, or coproduction, can happen in practice between patients, carers, and organisations and hopefully usefully bring a ‘reality check’ to the many conversations and debates that will take place over two days.
Working together or true coproduction is not as easy as it sounds in reality. Often I have found myself being used for a consultation or engagement event where I know that nothing I say will change anything and all that is really required by the organisation is an endorsement so that they can ‘tick’ the patient/carer/public engagement box.
That kind of exercise is so short-sighted as no one really gets anything positive from it- the organisation doesn’t get the insight they need to be really effective and for me, as a patient expert, all I’m left with if a feeling of frustration, having had my time and limited energy wasted.
I’m pleased to say my experience with EXPO15 and the Coalition for Collaborative Care, http://coalitionforcollaborativecare.org.uk
where I am a coproduction member, has been positively different. Specifically in the planning of the event:
- Patient/carer views were listened to seriously, discussed and acted upon;
- Proactive advice and suggestions were welcomed;
- Patient/carers were valued as equal members of the planning team.
Equally I have respect for the professionals who have key roles in planning such a high profile, national event with tight deadlines, a zero budget and small team. This is indeed evidence of developing better ways of true partnership and really working together from design to implementation.
It has been said that this year’s EXPO 2015 “..will be challenging, and will deal in reality not theory”. As a person who has Long Term Conditions I deal with the reality of that every day which includes chronic pain, limitations in mobility and lack of stamina on the negative side but also includes positive insight into personal resilience, into health and social care organisations and how simple changes could make big difference to people’s lives.
So I’m really looking forward to taking part in the two days in Manchester, my home city, on 2 and 3 September and particularly working in partnership with other members of the People’s Panel, the Coalition for Collaborative Care and the people I meet.
I’m looking forward to listening, learning and hopefully influencing too so that I can feel I have made a positive difference in the drive to ensure that true partnership working becomes embedded across health and social care so that person centred care can become a reality for everyone.
In other words the ‘get real’ factor – hope it helps.
Joining the dots
My first blog was written in March 2014 and was partly inspired by the NHS Change day initiative, which encourages individuals, groups and organisations to make a pledge for positive change. Now a year on I’m reflecting back and looking at new connections made since then.
The whole initiative really captured my imagination, as I firmly believe in the power of one individual to inspire others and then through connections and networks to set off a chain reaction for the better. 
This March 2015 Change day took place again and I made another pledge, which this year is to promote and share good
practice in patient experience in health and social care by using positively my personal experience as a patient with long-term conditions and my professional and voluntary connections. More detail can be found here.
http://changeday.nhs.uk/user_action/joining-the-dots/
I’ve recently, in February 2015, become a member of the co-production group of the Coalition for Collaborative Care (C4CC) where each person in the co-production group either has, or is a carer of someone with, Long Term Conditions. I’m hoping that together with the whole team at C4CC I can contribute to positive changes in the way health and social care is designed, delivered and evaluated for people with Long Term Conditions. For more details see:
http://coalitionforcollaborativecare.org.uk and https://twitter.com/Co4CC
As one lone individual, who can now only work part-time because of health issues, it can feel a bit isolating sometimes not having a substantive full-time role and function as I did in the past. But what keeps me going is the opportunity to identify and encourage more productive connections to be made within, across and beyond the different groups I work with in health and social care.
Using social media and Twitter in particular has for me opened up a wide breadth of possibilities in making new connections, strengthening existing ones and trying to be a positive catalyst for debate and change.
One very successful catalyst for positive change in health and social care is Gill Phillips who created Whose Shoes, a co-production tool to help people work together to improve lives, and who I met first on Twitter https://twitter.com/WhoseShoes
and had the pleasure of meeting in person quite recently in London.
Gill has also introduced me to the joys of Pinterest https://uk.pinterest.com and I found this poster on one of Gill’s board (now pinned on one of mine!), which made me think a bit more about this whole connections issue.
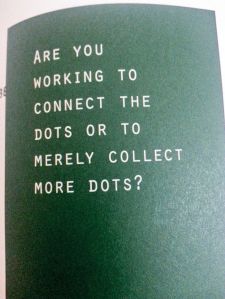
I’m connected to a number of health related groups and individuals through voluntary and Lay member roles in the NHS and if I mapped this out the page it would look quite busy but that’s not an end in itself and indeed could quite rightly be described as merely a ‘collection of dots’.
What is really important is what happens when the dots get connected or joined up such as for example when the North West NHS Lay members network meet up at Quarterly meetings and share information, ideas or discuss current topics and challenges.
But the story doesn’t end there as even though there is value in doing all of those things together, ‘dots’ sharing and thinking things through as it were. It is what happens when people go back to their own organisations and use what they have learned, digested or thought about to inform decisions and make changes that will improve health services for others that will make the biggest positive difference.
I’m now looking at all the ‘dots’ I’ve collected and seeing if I’ve made or enabled productive connections and what is happening or could happen because of those connections.
In the same way on the NHS Change day website they want to hear about actions that are taking place following people’s pledges or undertakings this year so that they can be shared and inspire others too.
So are you joining the dots and enabling positive connections in whatever you do?
And finally are you using your wider connections to share what you’ve done and inspire others? I’d love to hear about what you’ve done and share it.
Check out your dots-are they connected?
Social Media and healthcare conversations-it’s personal.
Social Media and healthcare conversations – it’s personal.
Before Christmas I was sharing my experience of using Social Media with NHS Lay Member colleagues at a network meeting in Manchester.

(a href=”http://www.freepik.com/free-photos-vectors/infographic”>Infographic vector designed by Freepik</a>)
Now I’m no communication expert, just an enthusiastic amateur, but fortunately at the meeting I did have a fellow colleague, George Wright, Digital Communications Manager at North West Commissioning Support Unit (NWCSU) who is, and who set the scene about how the use of Social Media and specifically Twitter has developed in the NHS.
George talked about how the NHS use of Twitter includes campaigns, information and engagement but that there has been a noticeable shift for many in healthcare to move from ‘broadcast to conversation’ and from organisations to individuals. A similar theme echoed in the title of Euan Semple’s book Organisations Don’t Tweet, People do. which makes for some useful reading.
My motivation and experience with Social Media was initially fuelled by a desire to keep up with my niece and nephew having been allowed to view their Facebook accounts. Having mastered that as an enthusiastic Internet user I was then curious to see what Twitter was about and gradually moved from re-tweeting to tweeting things myself to share with others.
My interests were largely based, but not exclusively, on healthcare, education and literature. Soon the penny dropped as I realised that Twitter was a global conversation opportunity that I could join in, meet new people, learn new things from and enjoy company with at any time of the day or night.
Conversations on Twitter about healthcare are usually driven by personal experience but as the NHS is such an enormous, complexity of organisations it can sometimes appear faceless which is odd as healthcare like most public services, is personal.
When it comes down to it if at anytime a person gets sick or injured it is an intense personal experience and could be the first time that person has needed any professional help.
Whoever you need to see for help whether that is a GP, nurse or Consultant it is a person, and a conversation will follow as to what happened, what the problem is and what might be the options to fix it or alleviate symptoms – person to person.
So it seems to me to make great sense for individuals who work in the NHS to actively use Social media not just as an additional tool to engage with people but to demonstrate that the NHS is about people first and foremost – a message that can sometimes get lost in pressured times.
Twitter has no boundaries or hierarchies, which I think is a good thing and very different from most NHS organisations, and is demonstrated if you ever get involved in a healthcare Tweetchat.
I joined in my first health Tweetchat last year in one run by the excellent wecommunities.org and founded by the then Agency nurse Teresa Chinn @AgencyNurse who you may have heard has been awarded an MBE in the recent New Years Honours list – Congratulations Teresa!

In my first Tweetchat there were 126 participants from around the world discussing Collaboration in commissioning. There were staff from NHS organisations, nurses, doctors, patients, Voluntary sector, private sector, other public sector organisations and members of the public all engaged in a frank exchange of views and ideas some of which is reflected in the word cloud below.
I would encourage anyone working in healthcare and particularly in the NHS to try out Twitter, if they haven’t already, and to join in a conversation or two.
I have met some amazing and interesting people and learned about what they are thinking and doing to make a positive difference in health and social care. Twitter has enabled these conversations and I enjoy taking part as an individual who happens to work and volunteer part time in the NHS and who is an active patient too.
Here’s a tiny snapshot of some of the people I’ve met through Twitter who are making a difference in health and social care.
- NHS England Project Manager Clare Helm @ClareHelm2 & supporter of @WeCommissioners along with David Foord @DGFoord, Dr Jonathan Griffiths @DrJonGriffths, Val Bayliss-Brideaux @Val_BB
- Dr Alys Cole-King @AlysColeKing who works so compassionately and positively in suicide prevention through http://www.connectingwithpeople.org
- Gill Phillips @Whoseshoes the inspirational developer of Whose shoes game used in dementia care and in the challenges of creating genuine personalised care support for people http://nutshellcomms.co.uk
- Helen Bevan @helenbevan Chief Transformation Officer NHSIQ founder of the The Edge, hub for change activist in heath & care
- Dr Kate Granger @GrangerKate founder of the inspirational #hellomynameis campaign
- David Gilbert @DavidGilbert43 and Mark Doughty @Patient Leaders Co-Directors’ & founders of Patient Leaders
Teresa Chinn MBE RN said in her Blog, Jan 2015 (www.teresachinn.co.uk ) that:
‘We should never underestimate the significance of starting a conversation that matters..’
And healthcare conversations are personal because they’re between and about people wherever they take place and can, and do, make a difference – even on Twitter.
____________________________________________________
Further information about using Social Media can be found at:
http://www.nhsproviders.org/news/analysis-of-social-media/
http://www.symplur.com/topic/patient-leadership/
Semple, Euan. Organizations don’t Tweet people do.- A Manager’s Guide to the Social Web. A John Wiley & Sons Ltd Publication 2012
or contact George Wright, Digital Communications/Corporate Manager at NHS North West Commissioning Support Unit (NWCSU) http://northwestcsu.nhs.uk george.wright@nhs.net or @georgewright19
Mental Health: Parity of Esteem- Rhetoric or reality
Have you ever visited your GP or A&E, been in excruciating pain that your doctor agrees is awful and which will definitely get worse without any urgent advice or treatment?
I must confess this has happened to me on numerous occasions as I’ve suffered broken bones, many slipped discs and a ruptured disc in my back – which was definitely off the 1-10 pain scale! – and had me shuffling slowly and painfully with sweat dripping off me until I’d been operated on.
On those and other occasions, which I won’t bore you with, when I suffered physical health problems I found the response of doctors and other healthcare practitioners to be pretty responsive, compassionate and keen to do something about the problem quickly.
But what a shock I had when faced with mental ill health 16 years ago and was diagnosed with severe clinical depression. I had subsequent recurring major episodes that endured for more than ten years. I now know I was ‘lucky’ to even get diagnosed and I have a GP to thank for that, who knew me well. I was also ‘lucky’ in being able to access psychological therapies and ‘only’ having to wait five months for that.
But I wasn’t so lucky in the following years when these episodes reoccurred or I hit crisis points. I discovered that services had been restructured since the last time I’d needed help, so the phone number I’d been given to call had been changed or someone had left.
Trying to navigate NHS structural and administrative changes when you’re feeling very ill is pretty difficult when you’re physically ill, but is almost impossible when mentally unwell.
Recovery for me was a slow and painful process, and I couldn’t have done it without professional help, medication, expert advice, mindfulness meditation and a strong support base of friends.
According to the Mental Health Policy group, who recently launched a Manifesto for Better Mental Health see here
“between 4,000 and 4,500 people take their own lives in England each year”.
Furthermore, “only a third of people with depression get any help, and even fewer get the full range of recommended NICE treatments.”
The report goes on to say that currently, “referrals to mental health services continue to increase. Monthly referrals to community mental health teams were up 13 per cent in 2013, and up 16 per cent for crisis services”. But money for mental health services has fallen in real terms.
I fully support the manifesto and the organisations who have come together to try to exert some influence in the mental health world and really hope that it is an additional lever to get some much needed improvements in mental health across the country.
I find it shocking that in 2014 mental health is treated differently to physical health and that access to the scarce range of treatments available is so poor. When I had broken bones I wasn’t asked to go home and wait for a number of months or years and then go back for treatment.
So why is it OK for someone with a severe mental health problem to be told to do just that?
I’ve never heard of anyone who was suffering from a life threatening physical problem, say a heart attack, who was locked up in police cell for safety because there was no medical help available?
Yet that happens frequently for people who are suicidal and in fact the police are often the only emergency service who offer help – so I’m not knocking them, just pointing out how truly shocking this is.
But what is more shocking to me is that we tolerate this state of affairs, as it has become the norm.
While the Parity of Esteem call to action by NHS England is welcome, I fear it will remain an aspiration that is never realised.
So what needs to be done?
Well, I think a seismic shift is urgently needed in commitment, funding and attitude to make any appreciable change in mental healthcare, which includes research, treatments and interdependencies with physical health.
This shift needs clear leadership at national, regional and local levels spanning government, NHS Commissioners, providers and the third sector.
No huge reviews need doing – just listen to the people who currently work flat-out in NHS mental health services and they will explain what’s needed.
Listen to charities such as Mind and Rethink, who do magnificent work helping people who are left without any access to treatments but have life-changing and life-limiting conditions.
Listen to the people who have lived life experience of mental health problems. Recovery is possible but many people never get the chance to find out.
Any new investment needs to be additional, designated finance and not become a contest for short-changing any other existing area of care.
Tolerating the norm is no longer an option – people’s health, quality of life and futures depend on the shift being made – and made quickly.
For further reading and evidence I recommend the report by the Royal College of Psychiatrists from March 2013- Whole-person care: From rhetoric to reality – Achieving parity between mental and physical health.







